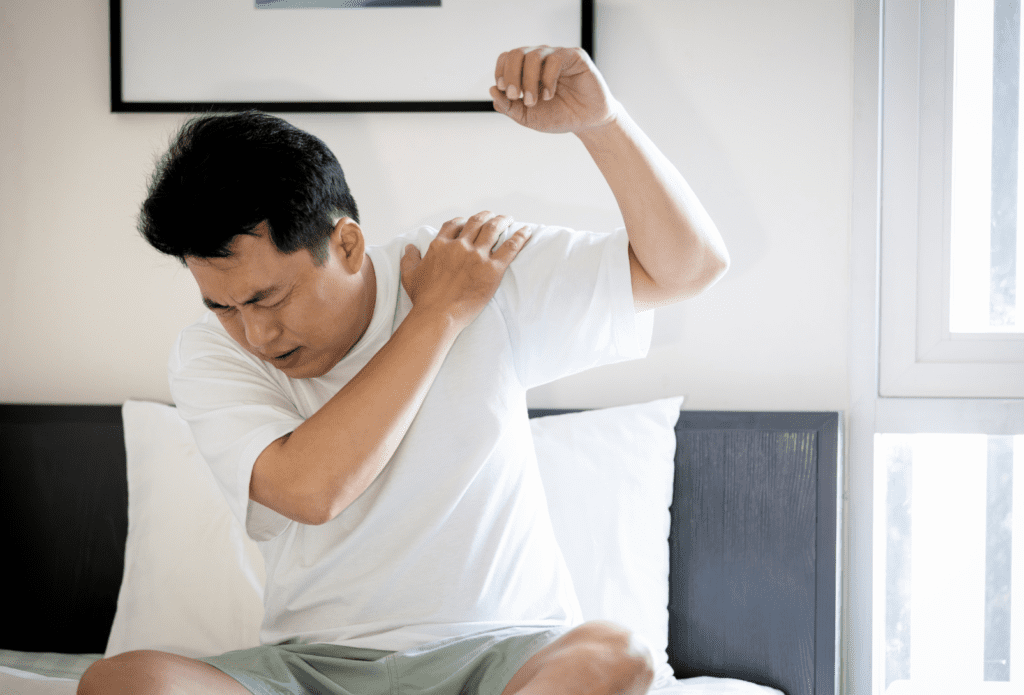
That sharp pinching pain when you reach overhead, behind your back, or even try to sleep on your side is classic shoulder impingement. If you’ve been told it’s simply due to “bad posture” or “upper crossed syndrome,” you’ve been given an oversimplified, and often unhelpful answer. At Redbird Wellness in Hopkins, we see impingement not as a single problem, but as a painful endpoint with several possible causes. Effective treatment starts by figuring out which combination is affecting you.
What’s Actually Happening When Your Shoulder Gets “Impingened”?
Impingement means something is getting pinched. In the shoulder, it’s usually the tendons of your rotator cuff or a bursa getting compressed under the bony arch of your shoulder blade (acromion). But the critical question, why is there excessive compression?
We systematically look for the real drivers which typically fall into four categories:
- True Mechanical Pinch: The space itself is physically narrowed.
- Muscle Dysfunction: Your rotator cuff isn’t doing its job to keep the ball centered in the socket during movement.
- Referred Pain: The pain feels like impingement, but the source is actually a stiff joint in your neck.
- Altered Movement: This is the most common culprit we find. Your shoulder blade isn’t moving enough, forcing everything underneath it to get crunched.
Why Shoulder Impingement Is Often a Load Tolerance Problem
Shoulder impingement is commonly described as a space issue, but space alone doesn’t explain why symptoms vary from day to day. A major driver is load tolerance. Tendons and bursae become painful when the demands placed on them exceed their current capacity. Sudden increases in overhead activity, repetitive lifting, or returning to workouts too quickly can overload tissues that aren’t prepared even if mechanics aren’t dramatically “wrong.” Lasting recovery requires rebuilding tolerance, not just creating space.
The Real Culprits: Look Beyond the Shoulder
Blaming “posture” puts the focus on a static position, but pain happens during movement. The problem is usually a lack of quality motion somewhere else. In our Hopkins clinic, we find the issue is almost never just in the shoulder joint.
#1 Cause: A Stiff Thoracic Spine (Mid-Back)
Your shoulder blade sits on your rib cage, which is attached to your spine. If your mid-back is stiff and can’t rotate or extend, your shoulder blade is forced into a poor position from the start and your shoulder blade will struggle to move all the up. Your body then compensates by overloading the shoulder joint, leading to pinching. This is our most common finding.
#2 Cause: Poor Shoulder Blade Control
Your shoulder blade is the foundation for your arm. If it’s weak, unstable, or moves out of sync with your arm (a dysfunction called scapular dyskinesis), it fails to create the necessary space for the rotator cuff tendons. The tendons then get repeatedly pinched.
This differs from the point above. The thoracic spine needs to extend and rotate so the shoulder blades have room to move and if it can’t the shoulder blades can’t do much. Shoulder blade control means the thoracic spine can do its job but now the shoulder blades themselves can’t move up, over, back, and down like they should.
#3 Cause: Neck (Cervical Spine) Stiffness
Nerves from your neck supply your shoulder. Irritation or stiffness in the lower cervical joints can refer pain directly into the shoulder, mimicking impingement. Many of the muscles that work on the shoulder and shoulder blade also work on the neck. If the neck has issues it will affect these muscles and then affect the shoulder. If we don’t check your neck, we might miss the true source.
Why Imaging Often Creates More Confusion Than Clarity
MRI and X-ray reports often list findings like bursitis, tendinosis, or bone spurs. While these sound concerning, they are extremely common in people with and without shoulder pain. Imaging shows what tissue looks like, not how it functions. Shoulder impingement is primarily a movement and load-management issue, not an imaging diagnosis. Over-reliance on scans can increase fear and delay meaningful recovery.
Night Pain, Sleeping Positions, and Shoulder Impingement
Shoulder impingement frequently worsens at night, especially when lying on the affected side. This isn’t because you’re “damaging” the shoulder in your sleep. Sustained compression and reduced circulation increase tissue sensitivity. Side sleeping with the arm internally rotated can further stress irritated tissues. Strategic pillow placement and daytime load management often reduce night pain without requiring complete rest.
The Redbird Approach: Create Space, Then Build Control
Our treatment follows a logical order. First, we create a better environment for the shoulder to move, and then we teach your body how to control it.
Phase 1: Decompress & Create Space
We often start with dynamic cupping around the shoulder blade and posterior shoulder. This decompresses the tight tissues that are pulling the joint into the impinged position, providing immediate pain relief and improving tissue mobility. This is our first-line tool to calm the area down.
Why Rest and Injections Often Fall Short
Rest and cortisone injections may temporarily reduce pain, but they don’t improve how the shoulder handles stress. Cortisone decreases inflammation, not dysfunction. When activity resumes without addressing movement capacity, symptoms frequently return. Long-term resolution of shoulder impingement requires progressive exposure to movement—not repeated shutdowns of symptoms.
Phase 2: Restore Motion & Build Resilience
This is where lasting change happens. Rehabilitative exercise is focused entirely on the true causes. We’ll prescribe movements to restore thoracic spine movement and teach you how to control your shoulder blade. The goal isn’t just strength. It’s retraining the coordinated movement patterns that protects your shoulder.
What Recovery from Shoulder Impingement Actually Looks Like
Recovery is rarely linear. Most people notice improvement in daily tasks first, followed by gradual tolerance to overhead movement. Temporary flare-ups are common and do not indicate failure. Understanding this timeline helps prevent fear-driven setbacks and keeps progress moving forward.
Phase 3: Address Specific Restrictions
As needed, we integrate other tools:
Chiropractic Manipulation: For stiff shoulder joints and spinal joints in the neck or mid-back.
MRT & Dry Needling: To release specific muscle tension in the upper back or rotator cuff that contributes to the dysfunctional pattern.
When It’s Probably Not Shoulder Impingement
Not all shoulder pain is impingement. Conditions like adhesive capsulitis (frozen shoulder), significant rotator cuff tears, or cervical nerve compression require different strategies. A thorough assessment ensures the right problem is being treated because even the best exercises won’t work for the wrong diagnosis.
Stop Chasing Posture, Start Building Better Movement
If you’re in Hopkins, Minnetonka, or St. Louis Park and tired of being told to just “fix your posture” or “rest your shoulder,” there’s a better way. We provide a clear assessment to find your specific impingement drivers and an active plan to resolve them.
Ready to move without that pinch? Schedule your shoulder impingement assessment at Redbird Wellness and let’s build a plan that addresses the root cause, not just the pain.
